
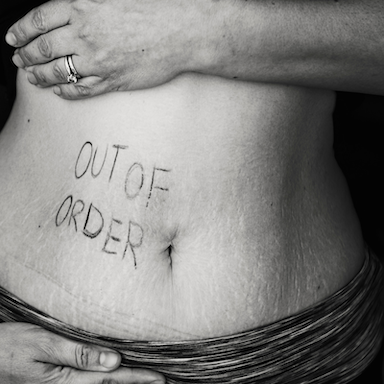
Is your IBS driving you crazy?
Bloating, gassy, cramps, heavy, uncomfortable? One minute you can’t go to the loo and the next minute you can’t get off it?
The likely cause is Irritable Bowel Syndrome (IBS). It’s incredibly common. According to Guts UK, a charity set up to promote awareness of and funding for digestive problems, it affects up to a third of people at some stage or another and it is one of the main reasons people visit their doctor.
Unfortunately, according to the NHS, there’s not a lot you can do. The official view is that it’s a lifelong problem that no one really understands and that there’s no cure for (although over-the-counter medicines can help symptoms). So sorry, move along and deal with it yourself.
As nutrition professionals will tell you, there IS hope. A consultation with a nutrition professional specialising in digestive health will be able to, in the first instance, provide some natural solutions that are likely better than taking over-the-counter medication AND your nutritionist will be able to work with you to find the root cause. This will enable you to get to the bottom of what is causing the symptoms of IBS (excuse the pun), and then you can take steps to fix it.
One of the most common causes of IBS is SIBO (small intestinal bacterial overgrowth), which accounts for 60##plus## of IBS cases. This describes a condition where bacteria manage to to grow and thrive in the small intestine. It’s not a question of ‘good’ or ‘bad’ bacteria. There shouldn’t really be many there at all.
It might be that you have a lactose intolerance. This is when your body is not able to tolerate lactose, a type of sugar found naturally in milk and other dairy products, leading to a host of ‘IBS symptoms’. It might similarly be fructose malabsorption. Again, some people are not able to absorb fructose and symptoms are very similar to lactose intolerance.
Dysbiosis is an imbalance in the levels of beneficial (good) and pathogenic (bad) bacteria in the large intestine or colon, potentially caused by the overuse of antibiotics or alcohol, an increase in high sugar diets, and stress.
Or you might have a yeast overgrowth. Simply, the gut environment gets out of balance (due to dysbiosis) such that unwelcome yeast can thrive.
None of these are pressing issues for regular doctors because there is often not the NHS testing or the framework for treatment of these problems. In some cases, digestive problems can be tricky to solve, and it almost always involves a lot of detective work. But if your symptoms are hampering your life in a significant way, I want you to know that there ARE things you can do. Although IBS might be very common, it is not normal to experience the symptoms you do.
What can I do about my IBS now?
There are some simple tricks you can put into practice today and that might make enough of a difference to help you get your life back on track. I’m going to tell you what they are in a moment.
I also want you to consider the degree to which your symptoms bother you. Are you satisfied with just covering up the symptoms and hoping for the best? That might be enough for you. If it isn’t, please book yourself in for a free 30-minute digestive health call to get an idea of what you can do right away and what might be possible for you.
10 ways to improve your digestion
The following suggestions are very basic but surprisingly effective at improving symptoms of digestive distress.
DO
DON’T
If you’re sick of feeling bloated, gassy, crampy or going to the loo too much (or too little), book in for a free 30-minute digestive health mini consultation. You can do that by clicking here.

THE MICROBIOME – HOW IT KEEPS US HAPPY AND HEALTHY
An adult human has around 2kg worth of microbes in our large intestine comprised of bacteria, viruses, archaea, fungi… and sometimes parasites. In fact, our guts are so well populated that we actually have more bacterial cells in our bodies than our own cells. And as odd as this may sound, this tiny ecosystem in our gut plays an essential role in our health and wellbeing, both physically and mentally.
When the bacteria in our gut are living in balance, with the right combination of good variety of types of bacteria, we have a wonderful symbiotic relationship with them, where we feed them fibre and, in return, they fulfil a number of roles for us:
Finally, our microbiome plays a key role in our mental health. This may be no surprise when you think about getting butterflies when you’re nervous or needing the loo when you’re frightened – the connection between our gut and our brain is very real indeed. Research shows that a happy gut is a happy brain and vice versa.
Sometimes called the Microbiome-Gut-Brain axis, the connection via the Vagus Nerve allows two-way communication between our brains and our guts, and scientists believe that this is to allow and monitor integration of gut signals into the emotional and cognitive centres of the brain. This allows our brains to have up-to-the-second information on our immune system, our gut function, plus production of certain gut-derived neurotransmitters, such as the feel-good serotonin. In turn, the brain supplies the gut with information to control immune function, motility and the permeability of the barriers.
Working alongside the central nervous system in such a way means that the microbiome and gut may have real influence over our emotional states, particularly when it comes to stress responses, anxiety and memory function. And this can often be seen in action with people with altered gut function, such as IBS, where other symptoms may include anxiety and low mood.
Looking after our microbiomes is therefore key to our overall health and mental wellbeing.
![]()
Please get in touch and find out more - I offer a free 30-minute exploratory call.