
Healthy, happy hormones
When you think about mental health, you’re probably thinking about your brain and how that works. The picture is often much more complex. Hormones play a big part because these chemical messengers are the background to everything that happens in your body. How you feel, therefore, is not just psychological, it’s biological.
Did you know, there are a huge number of symptoms that are common to both depression and hormonal imbalance? These include low energy, dizziness, low mood, apathy, anxiety, irritability, anger, lack of enthusiasm, despair, headaches, poor concentration, feelings of hopelessness, lack of confidence, low libido, fuzzy brain, memory loss, and insomnia (although there are others).
Rebalancing your hormones naturally is not something that happens overnight, but it can be greatly improved with the help of nutritional and lifestyle change. This blog will allow you to pinpoint where you might need help or support.
Mood and your cycle
Two of the main hormones that affect your feelings of mental wellbeing and clarity are oestrogen and progesterone, and these change throughout your menstrual cycle. It’s an over-simplification – but perhaps a helpful one – to think about oestrogen largely bringing positive effects to your mood and progesterone contributing more negative effects. With such a pronounced hormonal connection on mental health, it’s small wonder that women are twice as likely to suffer from depression than men.
According to the National Institute of Mental Health, 64% of women who suffer from depression say their symptoms get worse during the pre-menstrual period. Hormones are also likely to contribute to antenatal or postnatal depression, which affect around 10-15% of new mothers. And anxiety and depression are also starting to be recognised as symptoms of the peri- menopause on top of hot flushes and night sweats.
How it works
At certain times in your cycle (in the run-up to ovulation), there will be lots of oestrogen in your system and women tend to feel brighter and better in their mood. You might even notice at this time you feel better at talking and articulating yourself. In the second half of your cycle, oestrogen dips and progesterone comes into play. For some women, this can lead to lowered mood or depression.
PMS or PMDD
You might already experience this as Pre-menstrual Syndrome (PMS), a very common condition linked to the changing levels of these hormones, that might include feelings of bloating, breast tenderness or headaches, or manageable emotional symptoms like irritability.
For a small number of women (about 2-8%), the effect of these hormones on their mental wellbeing is pronounced. This is called Pre-menstrual Dysphoric Disorder (PMDD); an extreme form of PMS and one that, if you think might apply to you, you will want to ask your doctor about.
Why does this happen?
One of the first things to know is that the production of dopamine and serotonin (the two main brain chemicals associated with the development of depression and psychosis) is heavily linked to levels of oestrogen.
Research seems to suggest that there isn’t a noticeable difference in levels of oestrogen between those who are affected by mental health symptoms around their period or during the menopause – it seems some women are just especially sensitive to hormonal change, or perhaps also that lifestyle problems like stress may also play a big part.
Other hormones
Testosterone:
You might think of testosterone as the male hormone and, while men do produce much higher levels, every woman needs testosterone, too. Testosterone can increase sexual desire and libido, make bones and muscles strong, and have you feeling assertive and confident. The downside can be anger and aggression. If you suffer with PCOS, then you may be suffering from an excess of testosterone and other androgens, which comes with its own set of issues. Click here to find out more about this condition.
Thyroid:
Altered levels of thyroid hormones impact on mental wellbeing. If you just don’t feel like yourself, feel lethargic and low, it could be that your levels of active thyroid hormone are low. This can often run hand in hand with other types of hormonal imbalance, such as perimenopause or PCOS.
Cortisol:
Cortisol is one of the main stress hormones and, when stress levels are high, literally any of the mood-related symptoms I have mentioned in any of the above might be present.
Oxytocin:
Oxytocin directly opposes cortisol. It’s the love hormone and, if you have children, you might recognise it as the hormone that floods women after childbirth to encourage bonding. It has a direct effect on appetite, insulin resistance, weight loss – and your mood.
Impact of hormones on your blood sugar levels
Declining oestrogen levels have a role to play in insulin sensitivity (that means how sensitive – or not – the cells in your body are to the fat storage hormone insulin). In fact, a lack of sensitivity to insulin (or even being resistant to the effects of insulin) is lurking behind many of the common hormonal symptoms, particularly in menopause or PCOS, like fatigue and weight gain as well as symptoms of low mood like brain fog, anxiety and depression.
“Hormones and mental health” is a complex picture in which your physiological health and mental wellbeing are inextricably intertwined. It’s best to work with a nutrition practitioner to unravel this for you. They will be able to piece together a hormone balancing food and lifestyle plan to suit your circumstances. Check out my Hormone Balancing Action Plan or why not book in a call here?
Is it the Menopause?
Officially menopause is when you’ve gone for 12 months without a period at all which signifies the end of female reproductive capabilities. However, most symptoms occur in the 2-10 years leading up this – which is known as perimenopause.
Unfortunately, there's no specific blood test for perimenopause. And this is where a lot of confusion starts to arise. Many of my clients have odd symptoms which send them to the GP, only to realise a couple of years later that it was probably perimenopause…
I often use the DUTCH test, a dried urine test, which can be very useful in looking at a complete balance of sex and stress hormones during this turbulent time. While testing hormones during perimenopause and menopause is not often done in conventional medicine, understanding hormone levels and their metabolism (as well as assessing our stress levels) can help guide recommendations to support women during this stage in their life. Do get in touch with me if you’d like to discuss this further.
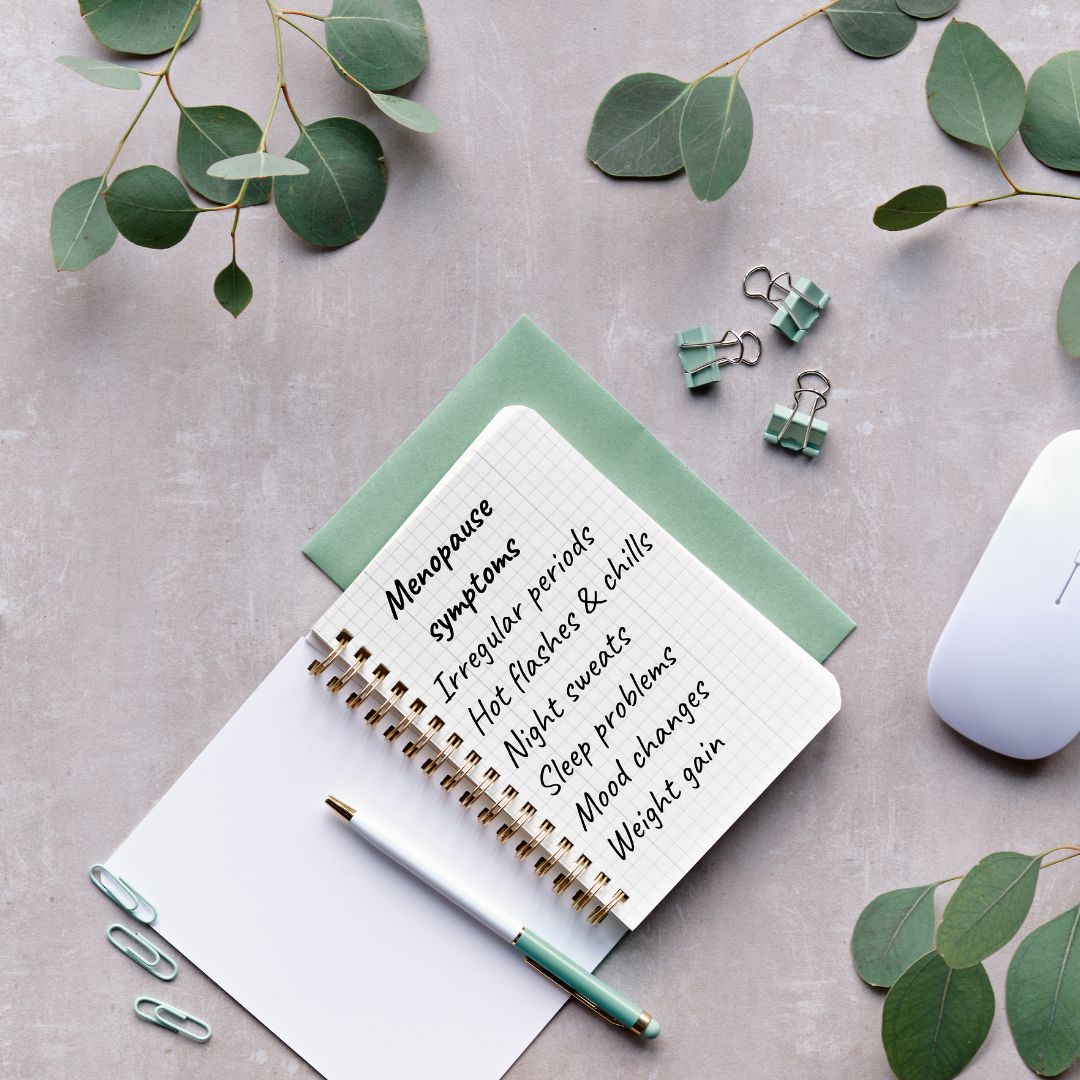
But what are the symptoms of perimenopause? Because our hormones affect our whole bodies, not just our sexual characteristics, perimenopause can bring a whole heap of symptoms with it, such as:
(Please note: some of these symptoms may not be perimenopause – so if you’re worried, do check with your GP!).
When and how we suffer tends to be based on a combination of genes, our health, and our environment. If you can, it might be good to ask your mum when she had hers and how it affected her. But, overall, it’s one helluva time. No wonder it’s sometimes called second puberty.
Most of the symptoms we have are due to fluctuating oestrogen and intermittent progesterone, brought about by the natural retirement of our ovaries.
Why is oestrogen so important?
Well, we have receptors to oestrogen all over our bodies – they’re not just responsible for the reproductive cycle. They are found in our brains, bones, guts – just about everywhere.
Oestrogen helps us build muscle, regulates bone density, and promotes healthy skin. It helps maintain healthy brain function. It looks after our heart and cholesterol levels. And it even has a hand in our gut function. But probably most noticeably is abdominal weight gain or ‘menobelly’. This is where we start to gain weight around our middles that we possibly didn’t have before, and it’s now more difficult to get rid of too.
So, how do you know if you’re in menopause?
As a rule of thumb, we can tell that it’s probably perimenopause if you’re having:
or
If you’re still not certain, check in with your GP or nurse, or book in a free call with me here at the clinic.
Food to Fix Your Hormones
PHYTOESTROGENS
What are they and why you need them.
When it comes to diet, food is so much more than macronutrients like protein, carbohydrate and fat. And even more than the sum of its vitamin and mineral content. Some of the magic ingredients the nutrition world is talking about are phytoestrogens.
These are naturally occurring plant-based chemicals, which are structurally similar to oestrogen and exert a weak oestrogenic effect. The great news is that you can use them to gently help rebalance your hormones.
Phytoestrogens are particularly helpful for women because they are adaptogens. This means they can either replicate or counteract the effects of oestrogen. They’re useful for all women but especially if you are going through the perimenopause, have endometriosis, fibroids or PMT (any symptoms at all during or in the run up to your period).
HOW THEY HELP
Perimenopause
This is a stage in a woman’s life usually starting in her late 40s. During this time, your body stops making as many female hormones like oestrogen. This transitions into a time when your periods have stopped for at least 12 months – menopause. There are many uncomfortable symptoms that usually occur during this phase of your life, ranging from hot flushes and mood swings to decreased libido. Research shows that phytoestrogens can have a positive impact on many of these symptoms.
Bone health
Oestrogen plays an important role in maintaining bone mineral density. Osteoporosis is a disease in which bone density and quality is reduced, resulting in greater porosity of bones and a higher risk of fracture. Research is ongoing in this area but the work shows that a diet that brings these phytoestrogens into your life may help prevent osteoporosis.
Menstrual irregularities
Many menstrual problems are linked to too much oestrogen in your system – like endometriosis and fibroids. Phytoestrogen-rich foods decrease the effects of oestrogen levels naturally by blocking the oestrogen receptors on the cells in fibroids and other oestrogen-sensitive tissues.
Acne
Adult acne can result from an imbalance in hormones, often where male hormones like testosterone are present in a higher than normal ratio compared with oestrogen. The idea is that these plant sources of oestrogen counteract the effect of the male hormones and may help prevent acne as a result.
The Power of Food
While synthetic oestrogens (think HRT) have been linked to unfavourable outcomes like increased risk of some hormone-driven cancers, there are no known health risks from eating more plant foods.
Phytoestrogens and the gut
The absorption of phytoestrogens depends on a healthy gut, as there must be enough healthy bacteria to convert phytoestrogens into their active form. A probiotic supplement will be helpful here.
Phytoestrogen-rich foods:
The three types of phytoestrogens are isoflavones, lignans and coumestans
ISOFLAVONES
* Soybeans (and related products like tofu, tempeh, miso)
Edamame beans
Lentils
Beans (blackbeans, aduki beans, broad beans, pinto beans)
Chickpeas
Split peas
Alfalfa
Broccoli
Cauliflower
LIGNANS
* Flaxseeds
Sesame seeds
Sunflower seeds
Pumpkin seeds
Kale
Broccoli
Cabbage
Brussels sprouts
Fennel
Onion
Garlic
Apples/pears
Carrots
Asparagus
Wheat
Barley
Rye
Rice
Oats
Lentils
COUMESTANS
Split peas
Pinto beans
Alfalfa
Soybean sprouts
* denotes particularly rich source

Is histamine intolerance causing your symptoms?
What you eat and your health are a fantastically complicated puzzle. For so many reasons linked to modern living, some foods can disagree with you. You may already experience this directly. People with digestive problems can often point to specific foods causing upsets and, if you think you have a food intolerance, you might already suspect wheat, dairy, yeast, eggs, or any number of foods to be the culprit lurking behind your symptoms.
There’s one often-overlooked component found in some foods that you might not know about yet that I want to talk about today. Could it be this that’s causing you problems?
Histamine…too much of it for your body
If you have an allergy, you might already know about histamine since you probably take antihistamines to try to neutralise the effect is has on the body. Histamine is a signalling molecule that has a lot of roles in the body like making stomach acid and keeping you alert. It is also involved in the immune response and protects you from foreign invaders.
When your immune system spots a potential invader, one type of immune cell (your B cells) to make IgE antibodies and these are a bit like warning signals to other immune cells to tell them to be on alert. When they meet the ‘invader’, other immune cells (this time your mast cells and basophils) throw out histamine and other inflammatory chemicals to neutralise the attack.
This works really well for some types of invader - like parasites, as an example – but not so much when the system overreacts to harmless substances like peanuts, pollen, animal hair. Welcome to the common allergy. It’s a histamine thing. And, if you have an allergy, you might be well used to antihistamines that can block or dampen the effect of this kind of allergic response.
If you’re reading this thinking, this doesn’t concern me as I don’t have an allergy, here’s why you should be interested. Histamine can be a problem for many other people – especially women since there is a big link between oestrogen and the cells that release histamine.
Histamine symptoms tend to track with your menstrual cycle, peaking when oestrogen is at its highest and then again before your period. If you experience any of these symptoms, histamine could be the culprit:
This is because oestrogen stimulates the mast cells to make histamine while at the same time downregulating an enzyme called that breaks down histamine, diamine oxidase (DAO). As a triple whammy, histamine triggers the ovaries to make more oestrogen. This can result in oestrogen dominance, where oestrogen is present in the wrong ratio to other hormones.
Histamine problems can also be a feature of perimenopause due to erratic release of oestrogen. Although oestrogen levels are dropping rapidly, progesterone falls faster, leaving oestrogen unopposed.
Why do some people suffer, and others don’t?
Dealing with histamine problems
One of the things you can do to manage histamine problems is reducing foods that either contain histamine or are ‘histamine liberators’.
Which foods contain histamine?
These foods, while they don’t contain histamine, trigger the release of histamine:
And alcohol and black or green tea interfere with the enzymes needed to break down histamine.
Improving your gut health is always worth doing since do much of your health relies on a healthy gut. If you’ve been ignoring symptoms, especially if you think you have irritable bowel syndrome (IBS), we should talk. Getting your digestive system back into balance pays dividends for all aspects of your health.
Inflammatory foods like gluten, dairy, sugar and processed foods make the situation worse, encouraging the body to release inflammatory cytokines and histamine.
At the same time, increase anti-inflammatory foods. An easy way to do this is to add herbs and spices into your cooking. Particularly helpful ingredients include ginger, thyme, oregano, basil, chamomile, and turmeric
Support oestrogen detoxification by eating plenty of cruciferous veggies like broccoli, cauliflower, cabbage, Brussels sprouts
If you experience any of the symptoms I’ve talked about here, please do get it touch. It’s very easy to read things like this or take advice from Dr Google and end up following a very restrictive diet when this is not always necessary. Working one-to-one with a nutrition professional means that you can take advantage of their years of study to find a programme that helps support your health without overly restricting what you eat. It’s a minefield out there!

Here are my top five nutrition tips for helping to balance your hormones
If your hormones are out of whack or you struggle with anything to do with your mood, the very first thing to do is to take a good look at your diet and consider how much ‘real food’ you eat and how much of your diet is processed. If you switched to ONLY real food, making everything from scratch, you would see a big improvement in your health. Ready to do more?
Fruit and vegetables are packed full of nutrients compared to many other foods and are beneficial for all aspects of health. Focus on the low-sugar fruits (the ones that grow in this country ahead of tropical fruits like bananas, mango and pineapple). For veg, eat more of the stuff that grows above the ground as – as a general rule – it contains less starch and keeps blood sugar levels stable.
Choose a good source of protein at every meal and snack. Protein is needed for growth and repair in the body. Good sources of protein include eggs, organic meat and poultry, oily fish like wild salmon, trout, etc. and Greek yoghurt, nuts and seeds.
Carbohydrates can be broken down into simple carbs and complex carbs. In simple carbs, the sugar molecules that occur either naturally or as a result of added sugar are quickly digested and absorbed into the bloodstream. Examples of simple carbs are cakes, cookies and pastries (in fact, anything with sugar), white bread, rice and pasta, and potato. The result is you get a short-term high but afterwards you feel more tired, fuzzy-headed and hungry. Complex carbs are made up of hundreds of sugar molecules, and these are absorbed much more slowly so they keep you feeling fuller and focussed for longer. Focus on bringing more of these into your diet ahead of simple carbs. They include brown rice, oats, beans, chickpeas and lentils, quinoa, sweet potato.
Healthy fats are an essential part of a good diet and should not be seen as the enemy. Fats are also the building blocks of all hormones and keep cell membranes and nerve cells healthy. The best sources of fat are flaxseeds (also known as linseeds), avocado, olive oil, coconut oil, oily fish like wild salmon, nuts and seeds.
And don’t forget about sleep, movement, and stress relief when you’re looking at hormones! These are just as important as nutrition. If you’d like to know more, why not get in touch and see how I can help you.

When you think about mental health, you’re probably thinking about your brain and how that works. The picture is often much more complex. Hormones play a big part because these chemical messengers are the background to everything that happens in your body. How you feel, therefore, is not just psychological, it’s biological.
Did you know, there are a huge number of symptoms that are common to both depression and hormonal imbalance? These include low energy, dizziness, low mood, apathy, anxiety, irritability, anger, lack of enthusiasm, despair, headaches, poor concentration, feelings of hopelessness, lack of confidence, low libido, fuzzy brain, memory loss, and insomnia (although there are others).
Rebalancing your hormones naturally is not something that happens overnight, but it can be greatly improved with the help of nutritional and lifestyle change.
Mood and Cycle
Two of the main hormones that affect your feeling of mental wellbeing and clarity are oestrogen and progesterone, and these change throughout your menstrual cycle. It’s an over-simplification – but perhaps a helpful one – to think about oestrogen largely bringing positive effects to your mood and progesterone contributing more negative effects. With such a pronounced hormonal connection on mental health, it’s small wonder that women are twice as likely to suffer from depression than men.
According to the National Institute of Mental Health, 64% of women who suffer from depression say their symptoms get worse during the pre-menstrual period. Hormones are also likely to contribute to antenatal or postnatal depression, which affect around 10-15% of new mothers. And anxiety and depression are also starting to be recognised as symptoms of the perimenopause on top of hot flushes and night sweats.
How it works
At certain times in your cycle (in the run-up to ovulation), there will be lots of oestrogen in your system and women tend to feel brighter and better in their mood. You might even notice at this time you feel better at talking and articulating yourself. In the second half of your cycle, oestrogen dips, and progesterone comes into play. For some women, this can lead to lowered mood or depression.
You might already experience this as Pre-menstrual Syndrome (PMS), a very common condition linked to the changing levels of these hormones, that might include feelings of bloating, breast tenderness or headaches, or manageable emotional symptoms like irritability. For a small number of women (about 2-8%), the effect of these hormones on their mental wellbeing is pronounced. This is called Pre-menstrual Dysphoric Disorder (PMDD); an extreme form of PMS and one that, if you think might apply to you, you will want to ask your doctor about.
Why does this happen?
One of the first things to know is that the production of dopamine and serotonin (the two main brain chemicals associated with the development of depression and psychosis) is heavily linked to levels of oestrogen.
Research seems to suggest that there isn’t a noticeable difference in levels of oestrogen between those who are affected by mental health symptoms around their period or during the menopause – it seems some women are just especially sensitive to hormonal change, or perhaps also that lifestyle problems like stress may also play a big part.
Impact of hormones on blood sugar levels
Declining oestrogen levels have a role to play in insulin sensitivity (that means how sensitive – or not – the cells in your body are to the fat storage hormone insulin). In fact, a lack of sensitivity to insulin (or even being resistant to the effects of insulin) is lurking behind many of the common menopause symptoms, like hot flushes, fatigue and weight gain as well as symptoms of low mood like brain fog, anxiety and depression.
Hormones and mental health is a complex picture in which your physiological health and mental wellbeing are inextricably intertwined. It might be best to work with a nutrition practitioner to unravel this for you. We might be able to piece together a hormone balancing food and lifestyle plan to suit your circumstances. Get in touch if you feel you'd like to discuss this further.
![]()
Please get in touch and find out more - I offer a free 30-minute exploratory call.